Irritable Bowel Diseases
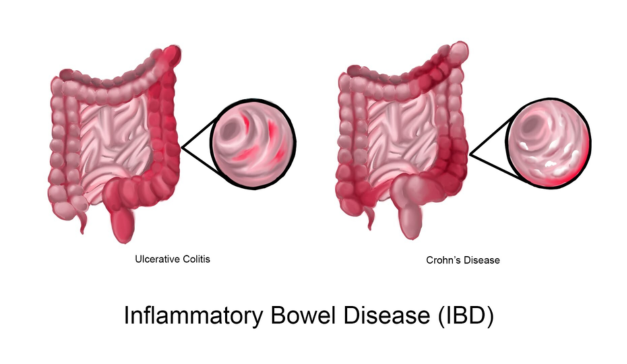
In the realm of managing Irritable Bowel Diseases (IBD) like Crohn’s Disease and Ulcerative Colitis, the Nutritional Therapy Functional Medicine Model emerges as a comprehensive and personalised approach. Unlike traditional medicine, functional medicine delves into the root causes of diseases,
offering tailored strategies to support individuals in their journey towards healing.
Understanding the Functional Medicine Approach
Functional medicine is a patient-centered model that emphasizes treating the whole person rather than merely addressing symptoms. It views the body as an interconnected system, recognizing the intricate relationships between genetics, environment, lifestyle, and nutrition.
The Four Pillars of Nutritional Therapy in Functional Medicine for IBD
1. Identifying Triggers and Root Causes
Functional medicine seeks to identify the triggers and root causes of IBD, understanding that each individual’s experience is unique. Through thorough assessments, including detailed medical history, genetic factors, and lifestyle habits, practitioners aim to unveil the underlying contributors to inflammation and gut dysfunction.
2. Personalized Nutritional Plans Nutritional therapy within the functional medicine model tailors dietary plans based on individual needs and responses. This personalized approach considers the specific requirements of patients with Crohn’s Disease or Ulcerative Colitis, acknowledging that certain foods may exacerbate
symptoms or contribute to inflammation.
3. Balancing the Microbiome
A key focus of functional medicine is restoring and maintaining a healthy gut microbiome. Probiotics, prebiotics, and dietary strategies are employed to foster a balanced microbial environment, promoting digestive health and mitigating inflammation associated with IBD.
4. Addressing Nutrient Deficiencies
Individuals with IBD often face challenges in nutrient absorption due to inflammation in the gut. Functional medicine practitioners address these deficiencies by implementing targeted nutritional interventions, ensuring that patients receive the essential vitamins and minerals crucial for their overall well-being.
Key Components of Nutritional Therapy in Functional Medicine
1. Testing the Microbiome via stool analyis
Functional medicine utilizes advanced testing, such as microbiome analysis, to identify specific bacteria, yeast or parasitic infections that may trigger inflammation or exacerbate IBD symptoms. Eliminating or minimizing these pathogens becomes an integral part of the personalized nutritional plan.
2. Inflammatory Modulation Through Diet
Functional medicine emphasizes the role of anti-inflammatory diets in managing IBD. This may include the incorporation of foods rich in omega-3 fatty acids, antioxidants, and anti-inflammatory compounds to support the body’s natural healing processes.
3. Lifestyle Modifications
Beyond diet, functional medicine recognizes the impact of lifestyle factors on IBD. Stress management, adequate sleep, and regular physical activity are integral components of a holistic approach to support the management of Crohn’s Disease and Ulcerative Colitis.
The Collaborative Journey to Healing
Collaboration is key in the functional medicine model. Patients work closely with practitioners to co- create a personalized plan that aligns with their unique needs and goals. Regular monitoring and adjustments ensure that the plan evolves with the individual’s progress and any changes in their health status.
Conclusion
The Nutritional Therapy Functional Medicine Model offers a dynamic and patient-centric approach to managing Irritable Bowel Diseases like Crohn’s Disease and Ulcerative Colitis. By exploring the root causes, addressing nutritional imbalances, and tailoring interventions, this model empowers individuals on their journey to healing. It is a paradigm shift that not only treats symptoms but aims to restore balance and optimize the body’s natural ability to heal itself.
What Our Clients Say About Us
I was diagnosed with Ulcerative Colitis in 2016. Once diagnosed I went into remission for about a
year. In late 2017 my symptoms came back and got worse and worse. The meds didn't seem to be
working anymore.
In March 2021 a doctors advised me to take an immunosuppressive drug (not great in the middle of
pandemic) and if that didn't work the next step would be to remove my colon!
My good friend recommended me to Emma and to be honest I was reluctant, as I had tried a
nutritionist the previous year with no benefit to my health. However, I thought I had nothing to lose
and gave it a go.
I met with Emma in March 2021 and with her support and advice (plus hard work from me) as of July
2022 I no longer have signs/symptoms of ulcerative colitis or anaemia and am leading a normal life
again. Thank you Emma
RishiIrritbale Bowel Disease
Our Partners





